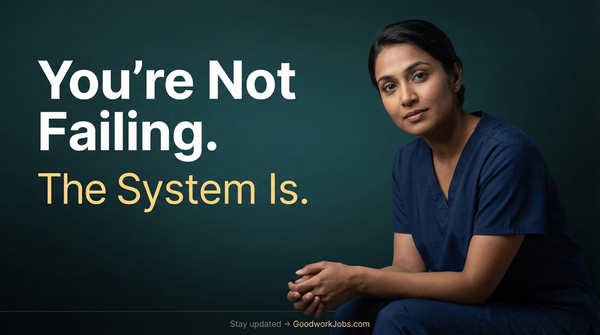
Compassion Fatigue in Nursing: What It Is and How to Deal With It

Understanding and Addressing Compassion Fatigue in Nursing
Compassion fatigue is a significant concern in the nursing profession, characterized by a gradual decline in empathy and emotional resilience. Recent studies indicate that approximately 25% of nurses experience high levels of compassion fatigue, underscoring the importance of recognizing and addressing this issue within healthcare settings.
What Is Compassion Fatigue?
Compassion fatigue, often referred to as the "cost of caring," manifests as profound emotional and physical exhaustion resulting from prolonged exposure to patients' suffering. This condition can lead to a diminished ability to empathize with patients, colleagues, and even loved ones.
Contributing Factors
Several factors contribute to the development of compassion fatigue among nurses:
- High Workloads: Extended shifts and staffing shortages increase stress levels.
- Challenging Work Environments: Exposure to trauma and critical care situations can be emotionally taxing.
- Limited Resources: Inadequate access to necessary tools and support hampers effective care delivery.
- Insufficient Compensation: Financial stress adds to overall job dissatisfaction.
These elements collectively impact nurses' well-being, leading to emotional exhaustion and reduced job satisfaction.
Compassion Fatigue vs. Burnout
While both conditions involve emotional exhaustion, they differ in origin and manifestation:Charlie Health
- Compassion Fatigue: Stems from continuous exposure to others' trauma, leading to a reduced capacity for empathy.
- Burnout: Results from prolonged workplace stress, characterized by feelings of hopelessness and inefficacy.
Understanding these distinctions is crucial for implementing appropriate interventions.
Recognizing the Signs
Early identification of compassion fatigue is vital. Common symptoms include:
- Persistent Fatigue: A constant sense of tiredness not alleviated by rest.
- Irritability: Increased frustration and mood swings.
- Reduced Empathy: Difficulty connecting with patients and colleagues.
- Detachment: Feeling disconnected from work and personal life.
- Physical Symptoms: Headaches, gastrointestinal issues, and sleep disturbances.
Recognizing these signs allows for timely support and intervention.
Strategies for Management
Addressing compassion fatigue requires a multifaceted approach:
- Organizational Support: Healthcare institutions should foster supportive environments, provide adequate staffing, and offer mental health resources.
- Education and Training: Programs like those offered by TEND Academy educate healthcare professionals on recognizing and managing compassion fatigue.
- Self-Care Practices: Encouraging activities such as regular exercise, adequate sleep, and mindfulness can bolster resilience.
- Peer Support: Establishing support groups allows nurses to share experiences and coping strategies.
Implementing these strategies can mitigate the effects of compassion fatigue and enhance overall well-being.
Compassion fatigue is a prevalent issue in nursing, impacting both caregivers and patient care quality. By recognizing the signs and implementing comprehensive support systems, healthcare organizations can promote a healthier work environment and ensure the sustainability of compassionate care.
For additional resources and support, visit GoodWork Health.